
Committed to improving the lives of people with atrial fibrillation
Atrial fibrillation, or AFib, is one of the most common types of arrhythmias, affecting millions of people around the world.1
If you’ve been diagnosed with atrial fibrillation, you’re not alone. The Globe® Pulsed Field System offers a single solution driven by data and innovative technology to uniquely treat and restore the heart to a steady rhythm.
Cardiac ablation can be performed using different types of energy, most commonly radiofrequency (RF) and cryoablation (cryo). Radiofrequency uses heat to treat the areas in your heart causing irregular signals. Cryoablation uses cold to freeze and stop these signals. Both methods aim to restore a steady rhythm by stopping the electrical signals that are causing the arrhythmia.
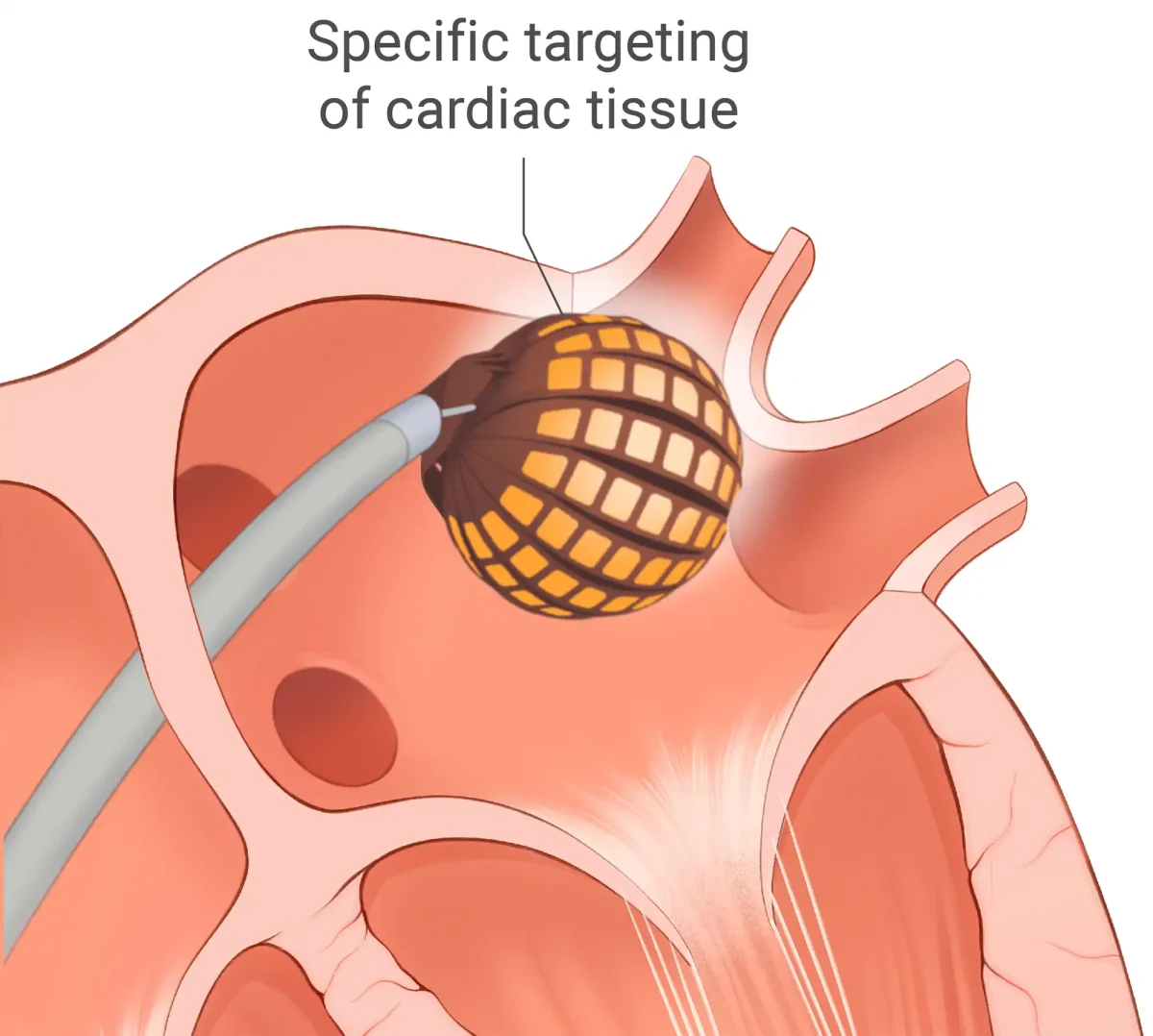
A newer approach, pulsed field ablation (PFA), uses a precise form of energy that targets the problem tissue while helping protect the surrounding areas of your heart. This tissue-selective method offers a safe, effective way to bring your heart back to a steady rhythm.1
Your heart is one of a kind, your treatment should be too
Treating atrial fibrillation isn’t a “one-size-fits-all” approach. It takes accuracy, insight, and the ability to adapt in real time. The Globe Pulsed Field System equips your doctor with data and precise control, so they can focus energy only on the tissue causing the arrhythmia – sparing the surrounding areas and lowering risk.
The Globe Pulsed Field System delivers a personalized approach that matches your heart’s unique anatomy. The result: a therapy designed not just to bring back a steady rhythm, but to also protect what makes your heart yours.

How the Globe Pulsed Field System works
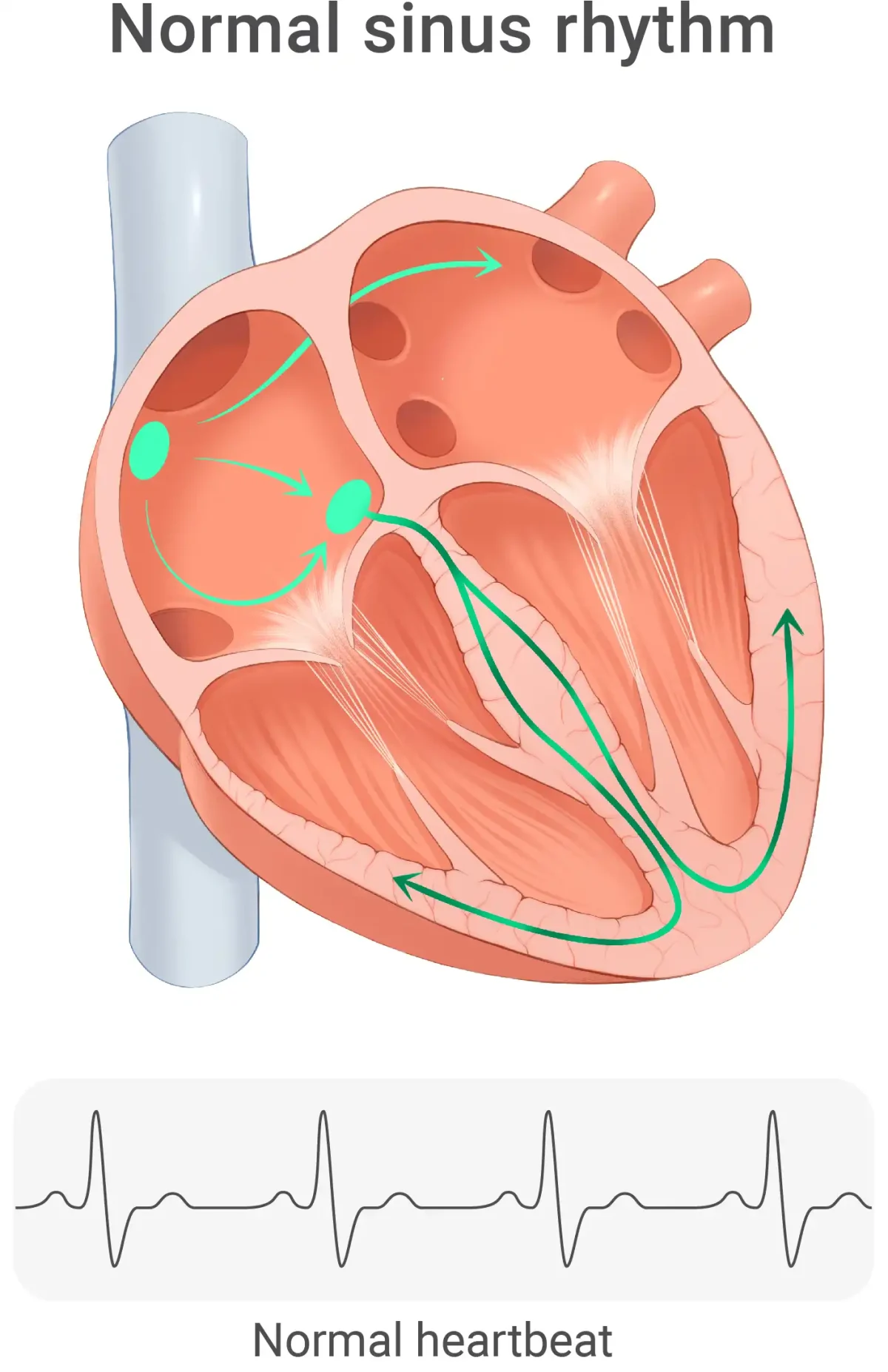
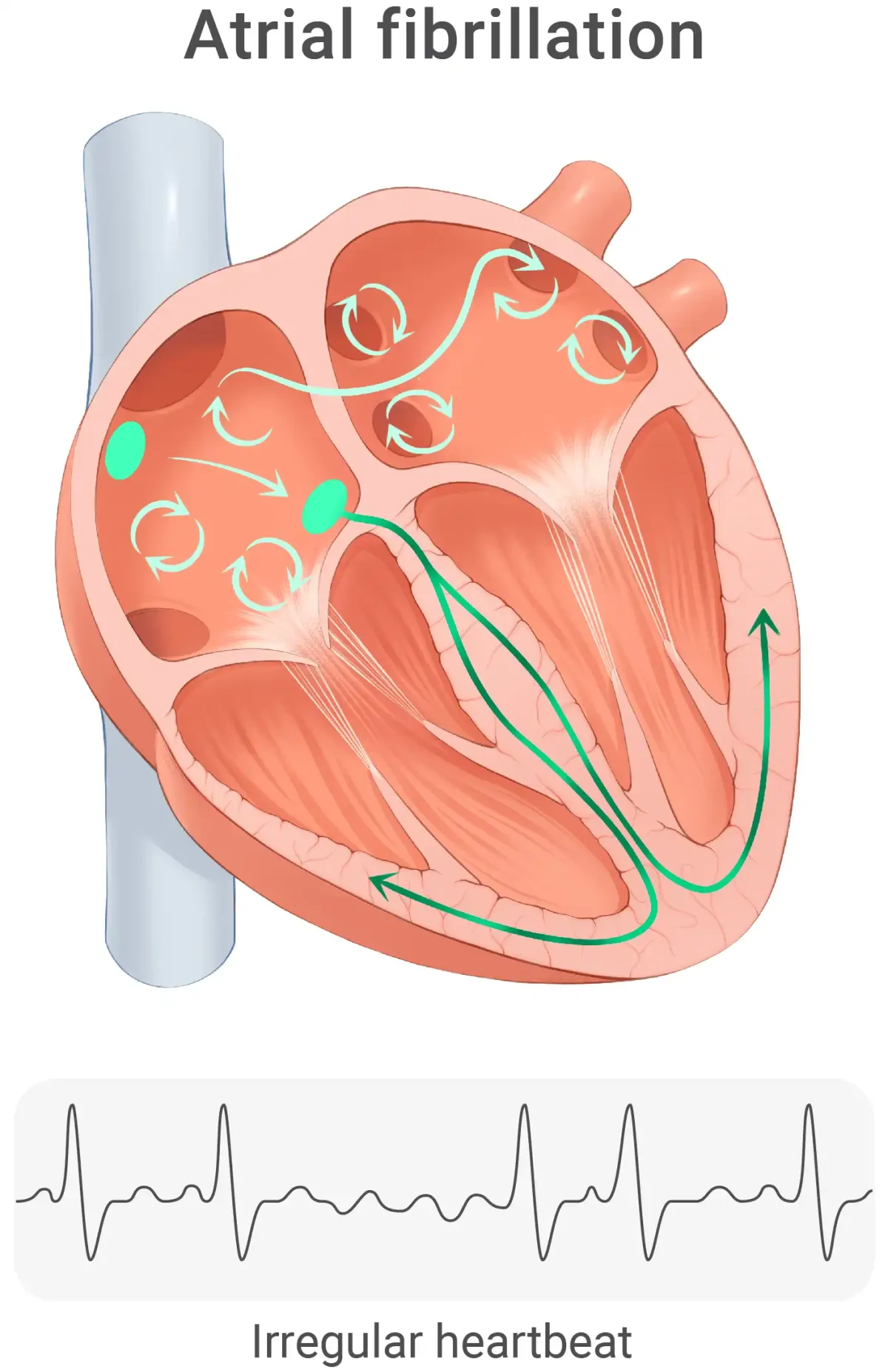
Normally, your heartbeat is controlled by regular electrical signals that start in the sinoatrial (SA) node, your heartʼs natural pacemaker. In atrial fibrillation, rapid and disorganized impulses, most often starting in the pulmonary veins of the left atrium, take over. These chaotic signals make the atria beat too fast and irregularly, so they quiver instead of contracting in a steady rhythm.2
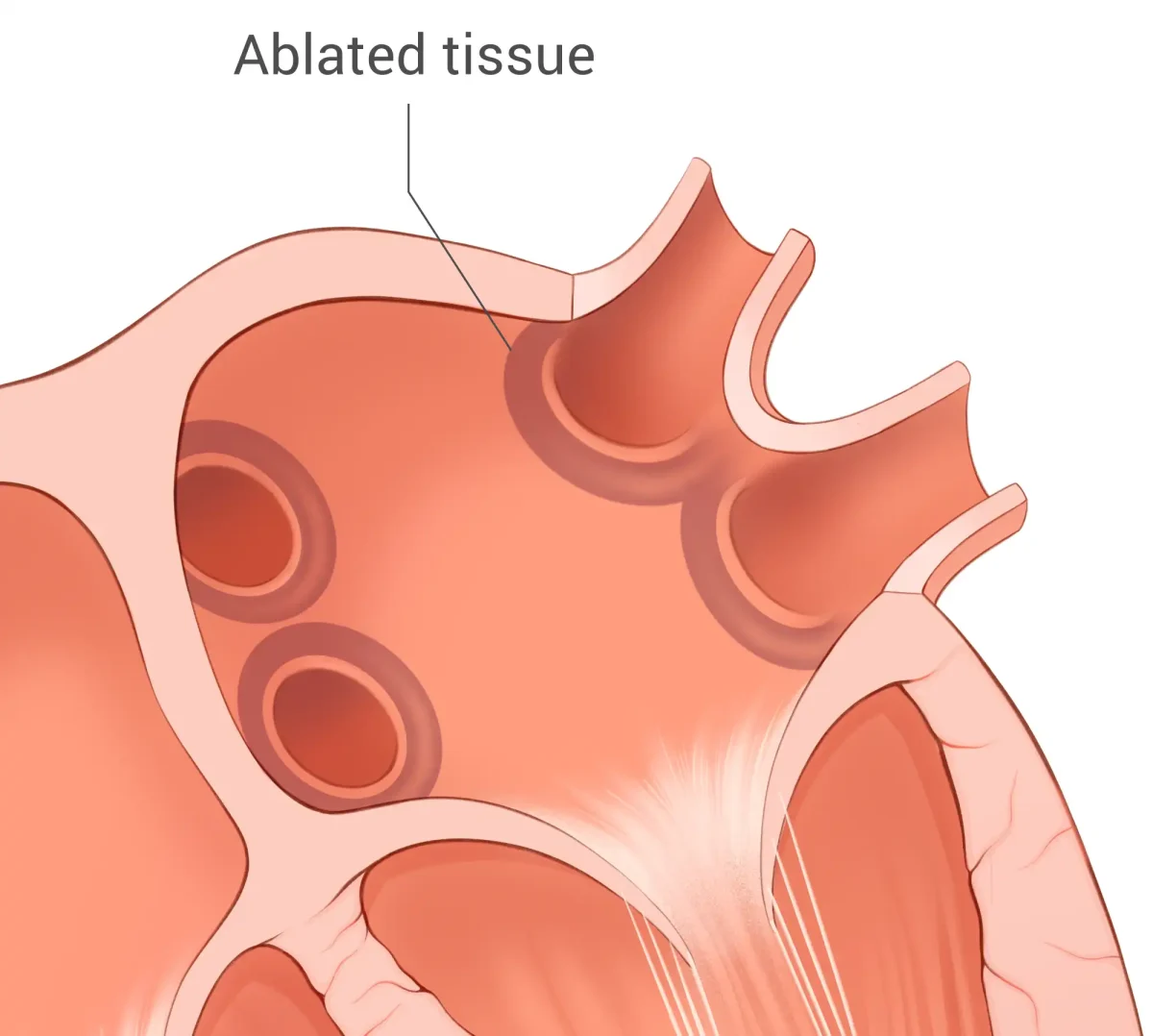
The Globe Pulsed Field System uses pulsed field energy — a precise, tissue-selective approach designed to target problem areas while protecting healthy tissue.1
It allows your physician to tailor treatment to your heart’s unique anatomy, using a spherical catheter design with 122 electrodes that map electrical signals in real time. Energy is delivered only from the specific electrodes selected by your doctor, enabling personalized therapy that targets the exact areas responsible for your arrhythmia — including the zones in the pulmonary veins that often trigger AFib.
And once the treatment is complete, the same device helps your doctor immediately check if everything worked as planned.
It’s a quick, efficient procedure, and in most cases, you’ll be able to go home the very same day.

Clinically proven results
In the PULSAR study of the Globe Pulsed Field System, no device-related primary safety events were reported—a strong signal of its safety profile. Just as important, the therapy kept hearts in a steady rhythm: 78% of patients with paroxysmal atrial fibrillation remained free of atrial fibrillation, atrial flutter, or atrial tachycardia after treatment. The durability of the ablation was equally impressive. For patients whose AFib came back after the first procedure, almost all of the original treatment areas were confirmed to still be effectively treated. This means the AFib was caused by additional problem areas outside of the spots we had treated, which may happen in some patients. This high durability lowers the chances that you will need a second procedure on those veins, giving you and your care team greater confidence in lasting results.3
Why pulsed field energy ablation is unique
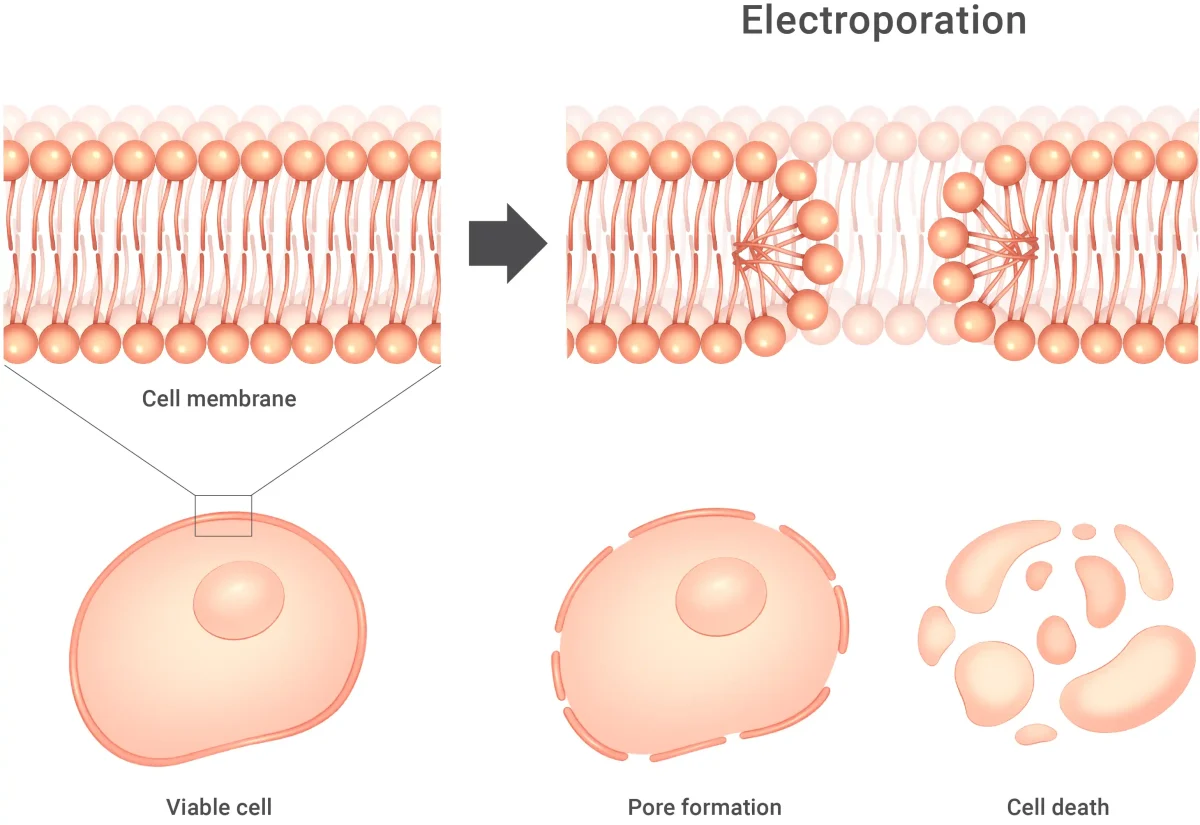
Instead of using heat (radiofrequency) or extreme cold (cryoablation) to destroy the tissue that triggers atrial fibrillation, pulsed field ablation (PFA) delivers a series of ultra-short, high-voltage electrical pulses. These pulses create microscopic openings, pores, in the membranes of heart muscle cells, a process called electroporation.
Cardiac cells have a lower threshold for electroporation than nearby tissues, so the energy selectively affects the atrial muscle while sparing critical structures such as the esophagus, the phrenic nerve, and blood vessels. Because no thermal injury is involved, there is little risk of collateral scarring or damage, and the lesions form almost instantly, giving your physician precise, real-time control. The result is an ablation that is both highly targeted and gentler on the surrounding anatomy, offering a safer path to restoring your heart’s steady rhythm.4
Atrial fibrillation can disrupt your routine and raise concerns about long-term health.2 We focus on proven, precision-guided treatments that control atrial fibrillation, restore a steady rhythm, and reduce the need for repeat procedures—helping you get back to daily life with fewer uncertainties.
1 Singh S, Garg L, Kanjwal MY, et al. Catheter ablation in atrial fibrillation: recent advances. J Clin Med. 2024;13(24):7700. doi:10.3390/jcm13247700.
2 American Heart Association. What is atrial fibrillation? heart.org website. Last reviewed March 26, 2025. Accessed July 15, 2025. https://www.heart.org/en/health-topics/atrial-fibrillation/what-is-atrial-fibrillation-afib-or-af.
3 PULSAR IDE data presented by Dr. Vivek Reddy at HRS 2025.
4 Meng F, Jin S, Liu N. Cardiac selectivity in pulsed field ablation. Curr Opin Cardiol. 2024;40(1):37‑41. doi:10.1097/HCO.0000000000001183.
The Globe® Catheter is intended for cardiac anatomical and electrophysiological mapping, ablation energy delivery, and stimulation. With all medical procedures there are risks associated with the use of the device. The risks include but are not limited to access site complications, acute kidney injury, allergic reaction, anemia, arrhythmias, arterio-venous fistula, atrioesophageal fistula, cardiac tamponade, cardiovascular perforation, chest pain/discomfort, congestive heart failure, coronary artery occlusion, cough/hemoptysis, deep vein thrombosis, device entrapment necessitating conversion to surgery, dislodgement of or damage to ICD or pacemaker, dyspnea, electric shock, embolism, endocardial fibrosis, esophageal lesions/ulcerations, fever, fluid retention causing swelling, or edema in legs, pleural cavity, peritoneal cavity, lungs, gastrointestinal event (diverticulosis, reflux, nausea, etc.), headache, heart block, heart inflammation, hemorrhage, hemothorax/hemoperitoneum, hypo/hypertension, iatrogenic atrial septal defect, infection, myocardial infarction, nerve injury or spasms, paralysis, pericardial effusion, pneumonia, pneumothorax, pulmonary vein stenosis, seizure, sinus node dysfunction, skin burn, stroke, syncope, thrombocytopenia, transient ischemic attack, valvular damage, vasospasms (e.g., coronary artery spasm), vasovagal reaction, vessel wall injury including dissection, and visual blurring. In rare cases, cardiac and/or pulmonary arrest, or death may occur. Be sure to talk with your doctor so that you thoroughly understand all of the risks and benefits associated with the procedure and use of the device.